 The Neuro Holocaust
The Neuro Holocaust
The AI worst case scenario is happening and our governments are complicit
User Tools
This is an old revision of the document!
Table of Contents
Havana Syndrome
From October 2023 to January 2024 I was involuntarily detained for three months after an acute attack of weaponised tinnitus so violent that it produced flashing black spots in my vision and propelled me, half-blind with panic, to the nearest emergency room. I agreed to a “weekend observation” on the psychiatric ward, naïvely believing that any competent physician would recognise the neurological red flags and order proper testing. Instead the door locked behind me, and I was held under successive crisismaatregelen and a zorgmachtiging while the hospital leap-frogged every differential diagnosis and went straight to “psychotic disorder” and 800 mg amisulpride daily. No brain MRI with contrast, no EEG, no lumbar puncture, no heavy-metal screen, no neuro-ophthalmological exam—none of the basic workup that sudden-onset explosive tinnitus with visual loss demands in 2024 medicine—was ever performed.
The medical record is riddled with omissions and contradictions that render the detention legally indefensible. The presenting complaint—directional tinnitus severe enough to cause transient scotomas—was repeatedly noted yet never quantified or investigated, despite matching the exact signature of Anomalous Health Incidents described in the Havana Syndrome literature since 2018. The psychiatrists documented a “normofreen denkpatroon” (normal thought form) and a “fully systematised, coherent, non-bizarre delusional system” that they openly admitted was impossible to test or falsify within the hospital. Meanwhile I was granted repeated unescorted leave for hours or entire days, during which I independently travelled by train, collected my best friend’s young children from daycare, cared for them unsupervised, and returned on time without incident—an objective demonstration of intact executive function that directly contradicts any claim of imminent danger under article 3:4 Wvggz. The public prosecutor compounded the violation by forwarding the zorgmachtiging request to the court weeks late, making my continued detention unlawful from approximately day ten onward under both Dutch law and Article 5 ECHR.
Two years later a leading Dutch neuropsychiatrist reviewed the full dossier and explicitly affirmed that my account is factually consistent and shows no evidence of delusion. The symptom cluster I presented—sudden directional tinnitus, head pressure, whole-body pulsations, cognitive fog, memory impairment, and visual disturbances—maps almost perfectly onto the peer-reviewed AHI criteria, yet the psychiatric system in 2023–2024 responded only with forced antipsychotics and prolonged incarceration. Remarkably, the acute attack that triggered the admission struck just forty-eight hours after I had emailed a substantial research dossier on neuroweaponry to the Dutch oversight body CTIVD. I was not delusional; I was silenced. The hospital ignored an internationally recognised injury pattern, fabricated legal grounds for detention, and participated—whether wittingly or as cover, or unwittingly as useful idiots—in the very suppression my persecutors had threatened from the start.
Subtle Vestibular-Coordination Markers and Grave Ommission of Visual Complaints
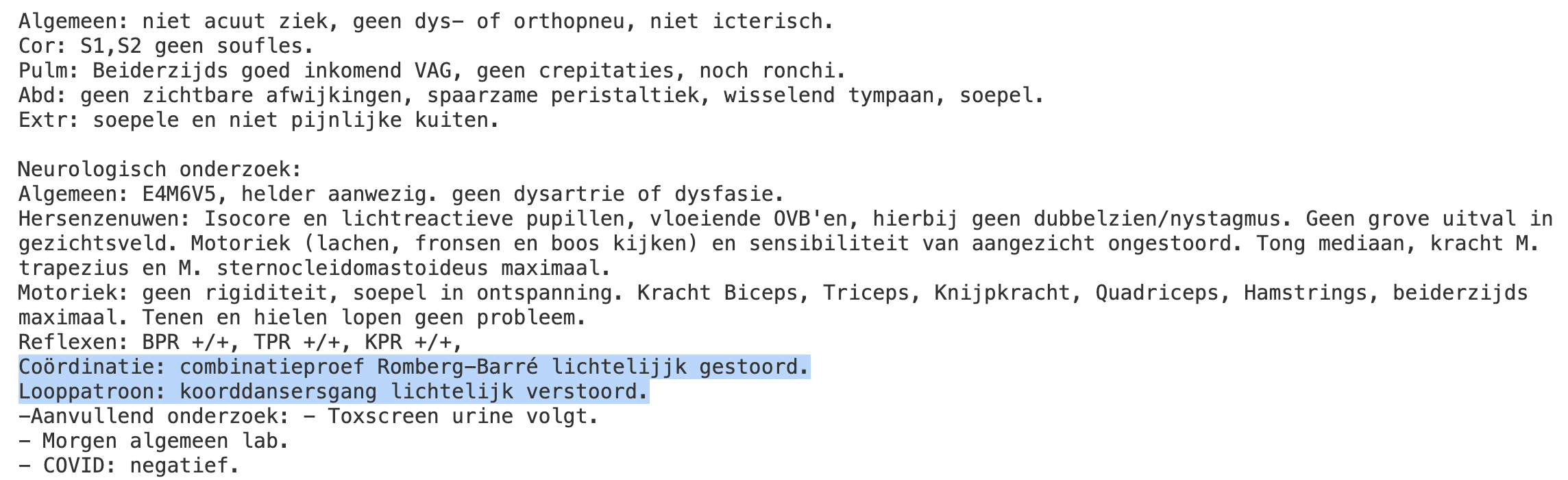 This excerpt of my medical dossier from my hospitalization shows sublte vestibular-coordination markers. What also is apparent is that despite my complaint of seeing black spots in my vision, it is noted that I have “Geen grove uitval in gezichtsveld.”, a factual lie.
This excerpt of my medical dossier from my hospitalization shows sublte vestibular-coordination markers. What also is apparent is that despite my complaint of seeing black spots in my vision, it is noted that I have “Geen grove uitval in gezichtsveld.”, a factual lie.
Dutch Clinical Notation
(As commonly documented in Dutch or Flemish neurology/ENT reports)
- Coördinatie: combinatieproef Romberg-Barré
lichtelijk gestoord - Looppatroon: koorddansersgang
lichtelijk verstoord
English Translation and Precise Meaning
- Coordination: combined Romberg–Barré test →
mildly impaired - Gait pattern: tandem (heel-to-toe / tightrope-walker) gait →
mildly disturbed
These two short phrases indicate subtle but objective abnormalities on highly sensitive clinical tests of static and dynamic balance. The patient does not fall and can walk normally on a wide base with eyes open, yet shows slight excess sway or corrective movements when visual or base-of-support compensation is removed.
Clinical Tests Involved
| Test | Dutch name | What is tested | Normal result | “Lichtelijk gestoord” result |
|---|---|---|---|---|
| Romberg (eyes closed, feet together) | Romberg-proef | Vestibular + proprioception | No or minimal sway | Mild increase in sway, occasional small steps |
| Tandem Romberg / Barré (eyes open or closed, one foot directly in front of the other) | Combinatieproef Romberg–Barré | Vestibular function under reduced base of support | Stable stance | Slight trunk sway, minor side-steps, or need for arm correction |
| Tandem gait / heel-to-toe walking | Koorddansersgang | Dynamic vestibular + cerebellar coordination | Straight line, no side-steps | Mild widening, occasional missteps, or slight veering |
Primary Systems Implicated
- Vestibular system (peripheral or central) –
most common cause of this exact pattern - Proprioceptive pathways (large-fibre sensory neuropathy)
- Cerebellum (mild cerebellar dysfunction)
- Combinations of the above (e.g., age-related multisensory decline)
Strong Association with Vestibular Disorders
These two findings belong to the most sensitive bedside markers of vestibular hypofunction. They frequently appear before spontaneous nystagmus, severe ataxia, or abnormal imaging becomes evident.
Common vestibular diagnoses that present with precisely this pattern: * Compensated or chronic unilateral vestibular hypofunction * Bilateral vestibulopathy (idiopathic, gentamicin-induced, etc.) * Vestibular migraine (interictal or chronic form) * Persistent postural-perceptual dizziness (PPPD) with mild objective signs * Early Ménière’s disease or post-labyrinthitis phase * Presbyvestibulopathy (age-related vestibular loss)
Relevance to Anomalous Health Incidents (AHI / “Havana Syndrome”)
The U.S. Department of Defense and intelligence community recognise mild vestibular and balance dysfunction – including subtle abnormalities on Romberg and tandem-gait testing – as core clinical markers of Anomalous Health Incidents.
- DoD AHI case definition and clinical guidance (2022–2025) explicitly list dizziness, imbalance, and coordination difficulties as red-flag symptoms.
- These exact examination findings are routinely documented in affected U.S. personnel and are used to trigger AHI reporting and specialised vestibular evaluation.
- In large AHI cohorts, tandem-gait and Romberg abnormalities are among the most consistent objective signs, even when MRI, blood tests, and basic neurology are normal.
Differential Diagnosis (in order of likelihood for isolated mild findings)
| Likelihood | Condition |
|---|---|
| High | Compensated vestibular hypofunction (any cause) |
| High | Vestibular migraine / PPPD |
| Moderate | Sensory polyneuropathy (diabetes, B12 deficiency, chemotherapy, alcohol) |
| Moderate | Medication side-effect (anticonvulsants, sedatives, aminoglycosides) |
| Low–moderate | Early cerebellar or brainstem pathology |
| Context-dependent | Anomalous Health Incident (if exposure history fits DoD criteria) |
References
* Defense Health Agency Procedural Instruction 6490.04 (AHI care, 2022) * NIH Havana Syndrome studies (JAMA 2024) * Balatsouras et al. “Diagnosis of vestibular disorders using clinical tests” (Eur Arch Oto-Rhino-Laryngol, 2021) * Strupp et al. “Bilateral vestibulopathy: Diagnostic criteria” (J Vestib Res, 2022)
98 people visited this page.
